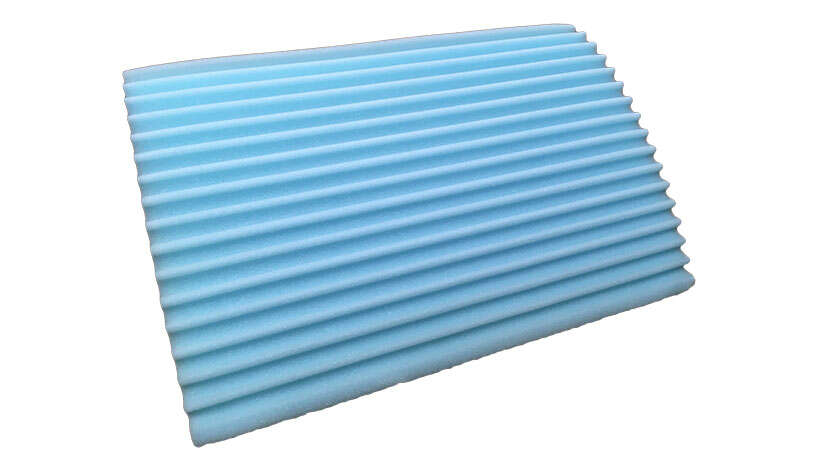
Conforming Comfort Patient Positioning Wedge
Although most hospital-acquired pressure injuries (HAPIs) are reasonably preventable,¹⁻⁴ approximately 2.5 million individuals in the United States develop a pressure injury in acute care facilities every year.⁵ These pressure injuries can result in extensive harm, including chronic wounds, and as many as 60,000 deaths annually. ⁶
HAPI care represents a substantial financial burden on health care systems. Previous estimates of the national cost of treating HAPIs ranged from $3.3 billion⁷ to $11 billion⁸ annually. In comparison, recent claims by Medicare beneficiaries showed that chronic pressure injury care accounted for about $22 billion.⁹ As the US Centers for Medicare and Medicaid Services (CMS) reduced reimbursement related to hospital-acquired conditions including HAPIs, hospitals have faced the full financial burden of these harms;⁸ ¹⁰ a single HAPI episode could cost hospitals anywhere from $500 to more than $70,000.¹⁻⁴
Incorporating turn and position wedges within your patient mobility program could potentially result in a reduction in pressure injuries. The use of mobility tools and patient positioning wedges can reduce friction and shearing on a patient’s skin, and can reduce moisture and pressure build up against a patient’s body.
References:
1. Duncan KD. Preventing pressure ulcers: the goal is zero. Jt Comm J Qual Patient Saf. 2007;33(10):605-610.
2. Berlowitz D, VanDeusen LC, Parker V, et al. Preventing Pressure Ulcers in Hospitals: A Toolkit for Improving Quality of Care. Rockville, MD: Agency for Healthcare Research and Quality; 2014.
3. Edsberg LE, Langemo D, Baharestani MM, Posthaur ME, Goldberg M. Unavoidable pressure injury: state of the science and consensus outcomes. J Wound Ostomy Continence Nurs. 2014;41(4):313-334.
4. Pham B, Stern A, Chen W, et al. Preventing pressure ulcers in long-term care: a cost-effectiveness analysis. Arch Intern Med. 2011;171(20):1839-1847.
5. Reddy M, Gill SS, Kalkar SR. Wu W, Anderson PJ, Rochon PA. Treatment of pressure ulcers: a systematic review. JAMA. 2008;300(22):2647-2662.
6. Bauer K, Rock K, Nazzal M, Jones O, Qu W. Pressure ulcers in the United States' inpatient population from 2008 to 2012: results of a retrospective nationwide study. Ostomy Wound Manage. 2016;62(11):30-38.
7. Van Den Bos J, Rustagi K, Gray T, et al. The $17.1 billion problem: the annual cost of measurable medical errors. Health Add (Millwood). 2011; 30(4):596-603.
8. Brenm H, Maggi J, Nierman D, et al. High cost of stage IV pressure ulcers. Am J Surg. 2010;200(4):473-477.
9. Nussbaum SR, Carter MJ, Fife CE, et al. An economic evaluation of the impact, cost, and Medicare policy implications of chronic nonhealing wounds. Value Health. 2018;21(1):27-32.
10. Centers of Medicare and Medicaid Services. Eliminating serious, preventable, and costly medical errors- never events. https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-Sheets/2006-FactSheets-Items/2006-05--18.html. 2006. Accessed February 22,2018.
11. Haesler E. Prevention and Treatment of Pressure Ulcers: Clinical Practice Guideline. Cambridge, UK: Cambridge Media; 2014.
HAPI care represents a substantial financial burden on health care systems. Previous estimates of the national cost of treating HAPIs ranged from $3.3 billion⁷ to $11 billion⁸ annually. In comparison, recent claims by Medicare beneficiaries showed that chronic pressure injury care accounted for about $22 billion.⁹ As the US Centers for Medicare and Medicaid Services (CMS) reduced reimbursement related to hospital-acquired conditions including HAPIs, hospitals have faced the full financial burden of these harms;⁸ ¹⁰ a single HAPI episode could cost hospitals anywhere from $500 to more than $70,000.¹⁻⁴
Incorporating turn and position wedges within your patient mobility program could potentially result in a reduction in pressure injuries. The use of mobility tools and patient positioning wedges can reduce friction and shearing on a patient’s skin, and can reduce moisture and pressure build up against a patient’s body.
References:
1. Duncan KD. Preventing pressure ulcers: the goal is zero. Jt Comm J Qual Patient Saf. 2007;33(10):605-610.
2. Berlowitz D, VanDeusen LC, Parker V, et al. Preventing Pressure Ulcers in Hospitals: A Toolkit for Improving Quality of Care. Rockville, MD: Agency for Healthcare Research and Quality; 2014.
3. Edsberg LE, Langemo D, Baharestani MM, Posthaur ME, Goldberg M. Unavoidable pressure injury: state of the science and consensus outcomes. J Wound Ostomy Continence Nurs. 2014;41(4):313-334.
4. Pham B, Stern A, Chen W, et al. Preventing pressure ulcers in long-term care: a cost-effectiveness analysis. Arch Intern Med. 2011;171(20):1839-1847.
5. Reddy M, Gill SS, Kalkar SR. Wu W, Anderson PJ, Rochon PA. Treatment of pressure ulcers: a systematic review. JAMA. 2008;300(22):2647-2662.
6. Bauer K, Rock K, Nazzal M, Jones O, Qu W. Pressure ulcers in the United States' inpatient population from 2008 to 2012: results of a retrospective nationwide study. Ostomy Wound Manage. 2016;62(11):30-38.
7. Van Den Bos J, Rustagi K, Gray T, et al. The $17.1 billion problem: the annual cost of measurable medical errors. Health Add (Millwood). 2011; 30(4):596-603.
8. Brenm H, Maggi J, Nierman D, et al. High cost of stage IV pressure ulcers. Am J Surg. 2010;200(4):473-477.
9. Nussbaum SR, Carter MJ, Fife CE, et al. An economic evaluation of the impact, cost, and Medicare policy implications of chronic nonhealing wounds. Value Health. 2018;21(1):27-32.
10. Centers of Medicare and Medicaid Services. Eliminating serious, preventable, and costly medical errors- never events. https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-Sheets/2006-FactSheets-Items/2006-05--18.html. 2006. Accessed February 22,2018.
11. Haesler E. Prevention and Treatment of Pressure Ulcers: Clinical Practice Guideline. Cambridge, UK: Cambridge Media; 2014.
• Single patient use wedges come with a non-woven cover that can be hand washed up to 3 times • Reusable wedge cover can be cleaned per facility’s disinfection instructions • Reusable cover has a non-skid fabric to help keep patient and wedge positioned according to facility’s protocol • Bariatric wedges are a dual density product with the bottom layer designed to support up to 500 lbs and comes standard with a memory foam top layer to address comfort and skin integrity
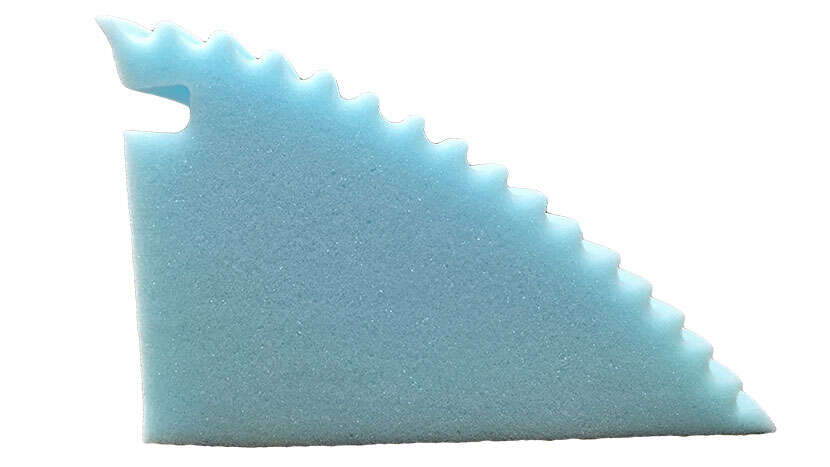
The 30° Conforming Comfort® articulated wedges aid in the prevention and treatment of pressure injuries by offloading the sacrum, while helping to provide proper body alignment. This design helps maintain a natural side lying position while providing improved comfort and support over the traditional flat-sided wedges, resulting in higher patient compliance. The articulated wedge design minimizes patient downward migration, hence reducing the need for boosting. Available in bariatric and standard sizes, and as a single patient use or reusable design.• Single patient use wedges come with a non-woven cover that can be hand washed up to 3 times
• Reusable wedge cover can be cleaned per facility’s disinfection instructions
• Reusable cover has a non-skid fabric to help keep patient and wedge positioned according to facility’s protocol
• Bariatric wedges are a dual density product with the bottom layer designed to support up to 500 lbs and comes standard with a memory foam top layer to address comfort and skin integrity
| Item Number | |
|---|---|
| Disposable, single patient use, Conforming Comfort® wedge cover. Bariatric use, SWL 500 lbs, 18” x 15” x 8” 12 ea/cs | |
| Wipeable Conforming Comfort wedge. Bariatric use, SWL 500 lbs, 18” x 15” x 8” 6 ea/cs | |
| Disposable, single patient use, Conforming Comfort articulated wedge. SWL 250 lbs, 18” x 10.5” x 7” 24 ea/cs | |
| Wipeable Conforming Comfort articulated wedge. SWL 250 lbs, 18” x 10.5” x 7” 12 ea/cs | |
| Disposable, non-woven cover fits standard wedge (item number LUS-WEDGE-SPU), standard size, 36 ea | |
| Disposable, non-woven cover fits bariatric wedge (item number LUS-WEDGEXLSPU), bariatric size, 36 ea | |