Kern County Hospital Authority - Arjo MOVE® Program
Safe patient handling, progressive mobility, pressure injury prevention and the key role of AirPal®
Kern Medical Center (“Kern Medical”), owned and operated by the Kern County Hospital Authority, is an acute care teaching center with 222 beds offering the only advanced trauma care between Fresno and Los Angeles, California. Kern Medical’s role as a safety net, public hospital places value on innovation adaptability. As a topflight regional health care system, Kern Medical is a leading voice for health, healing and wellness in the Central Valley.

The challenge
Prior to 2018, Kern Medical averaged 11 safe patient handling (SPH) injuries per year with an average annual worker’s compensation cost of $615,000. This resulted in an average of 152 lost days per year. In addition to the SPH injuries, reportable hospital acquired pressure injuries (HAPI) had reached 60 per year prior to 2018. Annually, pressure injuries (PIs) occur in more than 2.5 million US patients,1 of whom roughly 60,000 die due to infection or other complications,2 costing US healthcare more than $26.8 billion.3 PIs are difficult to prevent because injuries can develop quickly with irreversible damage occurring in vulnerable patients within a matter of hours.4,5
The impact of PIs to patients is substantial — reduced quality of life, high levels of pain, loss of independence, reduced mobility, and potential of leading to life threatening complications. Facilities incur longer length of patient stay, increased cost of treatment and nursing time, and litigation risk.6
Staffing constraints and the rise in obesity cause challenges to safe patient handling. Traditional techniques for moving a patient are physically demanding for caregivers.7 Despite the awareness of potential injury, 60% of caregiver injury remains from in-bed repositioning and lateral transfers.8 When working with patients of size, there is often a need for additional caregivers to participate in safe repositioning or transferring of a patient. Due to staffing challenges often, there are very few caregivers available to assist in moving these patients safely. As a result, there can be a risk for injury to the caregiver. In addition, patients may not be boosted, turned or repositioned according to plan this can place the patient at a high risk for a hospital acquired pressure injury (HAPI) due to immobility.9
Kern Medical faced the same challenges as the rest of the nation, including; high staff turn-over, high utilization of travel staff, inexperienced staff and staffing shortages. A desire to reduce caregiver injury prompted the use of air-assisted technology.
“Up Sooner Safe has been a tremendous success. It has contributed directly to a reduction in workplace injuries and mitigated the severity of incidents when they occur. By prioritizing patient care and ensuring employee safety, we create a secure environment where staff can focus on delivering quality care.”
Mauricio Cardona, Kern Medical Risk Manager
The approach
Kern Medical’s response to California AB1136 – The Hospital Patient and Health Care Worker Injury Protection Act, was a steadily evolving solution that met the requirements of the legislation but was limited due to the fiscal investment needed for a fully developed program. A safe patient handling (SPH) and progressive mobility program was long on the Kern Medical radar to equip staff with a patient-centered solution. Kern Medical was fortunate to receive a grant from Kaiser Permanente as a community partner that would fully fund Kern Medical’s Up Sooner Safer program. With this funding, the Progressive Mobility Committee was created and the evolution of the SPH/Progressive Mobility program, Up Sooner Safer began. The finished program took one-year of development. During development and gap-analysis, the Kern Medical’s CT Department was an area of focused attention.
Up Sooner Safer resulted in a policy-driven, full-scale SPH/Progressive Mobility program throughout the organization with the deployment of dependent lifts, stand-assist aides and lateral transfer/repositioning aides. Three policies were developed: a specific, safe patient handling policy; a general, progressive mobility policy (laying the groundwork); and a progressive mobility, standardized procedure policy (to make mobility the expectation, immobility the exception).
Radiology Departments are typically small, tight-knit communities. When discussing SPH, the Radiology Department is often overlooked. However, this specialized area is constantly moving patients with little assistance or attention.
CT Departments do not require extensive staffing to perform the imaging, but this presents limitations when performing the necessary lateral transfers onto and off the imaging tables, especially in the acute care, trauma hospital setting. In the acute setting, the CT technologist usually only has one additional person to assist with the transfer, regardless of the size of the patient. Previous methods involved the use of backboards and the poor body mechanics needed to lift and transfer a patient. The combination of repeated transfers, poor technique and limited staffing resulted in the Kern Medical CT department being a high-risk injury area. It was not enough to ask if a patient handling injury would occur, but rather when and how severe.
When looking within a Radiology Department, specifically Computed Tomography (CT), this department performs lateral transfers throughout every shift. Staffing challenges would often drive caregivers to perform tasks that put them at risk for injury. In the CT Department, there is no alternative to the lateral transfer needed to gain the imaging required. At Kern Medical, prior to the implementation of their SPH-Progressive Mobility program, it was found that CT staff would often ignore the aches and pains that frequently occur with the transfers of their patients for the ‘betterment’ of their department. According to staff, any missed days would result in short-staffing, decreased patient throughput and an increased burden on available CT staff.
Why AirPal?
During the vetting process in determining which mobility vendor Kern Medical would work with in developing Up Sooner Safer, Arjo was selected due to the clinical support offered, equipment-line available, footprint size of the equipment and ease of use. This included the AirPal. It was a natural fit to then incorporate it into our lateral transfer protocols/algorithm.
The AirPal is an air mattress technology that can remain beneath a patient. When the AirPal mattress is inflated, it gently raises the patient uniformly and allows the caregiver to reposition and laterally transfer a patient with significantly reduced friction. This ensures both the patient and caregivers are safe during patient transfer.
Implementation of Up Sooner Safer and AirPal
Like many forms of technology, AirPal is only effective if it is used appropriately. The successful implementation of any technology for SPH requires appropriate training to the product, as well as policies and procedures that encourage the continued use of the product. By establishing, a standard procedure for use of the AirPal consistent practice drove increased utilization and therefore compliance with the technology.
Up Sooner Safer, launched in December 2017, with much fanfare and deployment of equipment. Prior to the launch, every clinical department and nursing unit selected Mobility Coaches for hands-on training. One month prior to program launch, Coach training was coordinated between internal Staff Development and Arjo’s MOVE Program. The Mobility Coaches would serve as program and departmental resources to assist with training and education of non-coaches. Upon completion of Mobility Coach training, hands-on training of non-coaches then began, including RNs, PCT/CNAs, RTs, PTs, OTs, SLPs, Transporters, OR Staff and Radiology Staff. Hands-on training was completed house-wide within two-months. On-going, hands-on training continued upon hire and then annually. Through focused training and follow-up appropriate use of the AirPal attained a 100% compliance rate.
During the gap-analysis it was determined the CT Department would need ceiling lifts to be used in combination with lateral transfer devices. This would allow for safe transfer of outpatients and in-patients alike. As processes continued to be evaluated in CT department, uniformity was needed to ensure safety of staff and patients. The average annual CT scans performed at Kern Medical is over 25,000 (see Graph 1) with the use of two CT scanning machines. The majority of CT scans require lateral transfers of the patient, to and from the exam table. This resulted in policy that all patients coming to CT department have an AirPal already in place under the patient. The AirPal could remain under the patient throughout the CT scanning process. This simplified the processes for all staff involved. The alternative would mean staff choosing a sling (for the ceiling lift) or AirPal for CT scan. Variability to processes can lead to breakdown or non-compliance so the AirPal path was chosen due to ease of use, continued future use of the AirPal during inpatient stay and improved patient comfort using the AirPal in comparison to using the ceiling lift sling. The ceiling lifts continue to be used throughout a shift but have been found to be a better use for outpatients.
Graph 1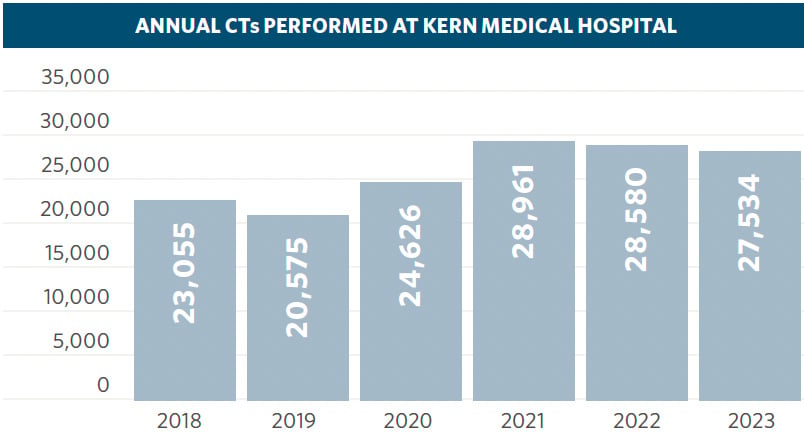
Since the Up Sooner Safer launch, the CT Department has performed over 150,000 imaging exams with zero patient handling injuries to caregivers. As one of the only Level II Trauma Center between Los Angeles and Fresno, Kern Medical’s trauma volume is very high. This steady admission rate results in high CT scanning volume. Trauma patients, once stable are sent to the CT department for imaging. After the introduction of Up Sooner Safer, ongoing gap-analysis found that these trauma patients were not a part of the AirPal placement for CT. Instead, these patients continued to be laterally transferred with slide-boards by CT department and emergency department (ED) staff. Through trial and analysis, an algorithm was developed in which an AirPal is placed on the ED gurney prior to trauma patient arrival. If suspected injuries are contraindicated (spinal precautions) to inflate the AirPal for CT scan, the AirPal is used uninflated until imaging clears the suspected injury for AirPal inflation. (see Algorithm)
Algorithm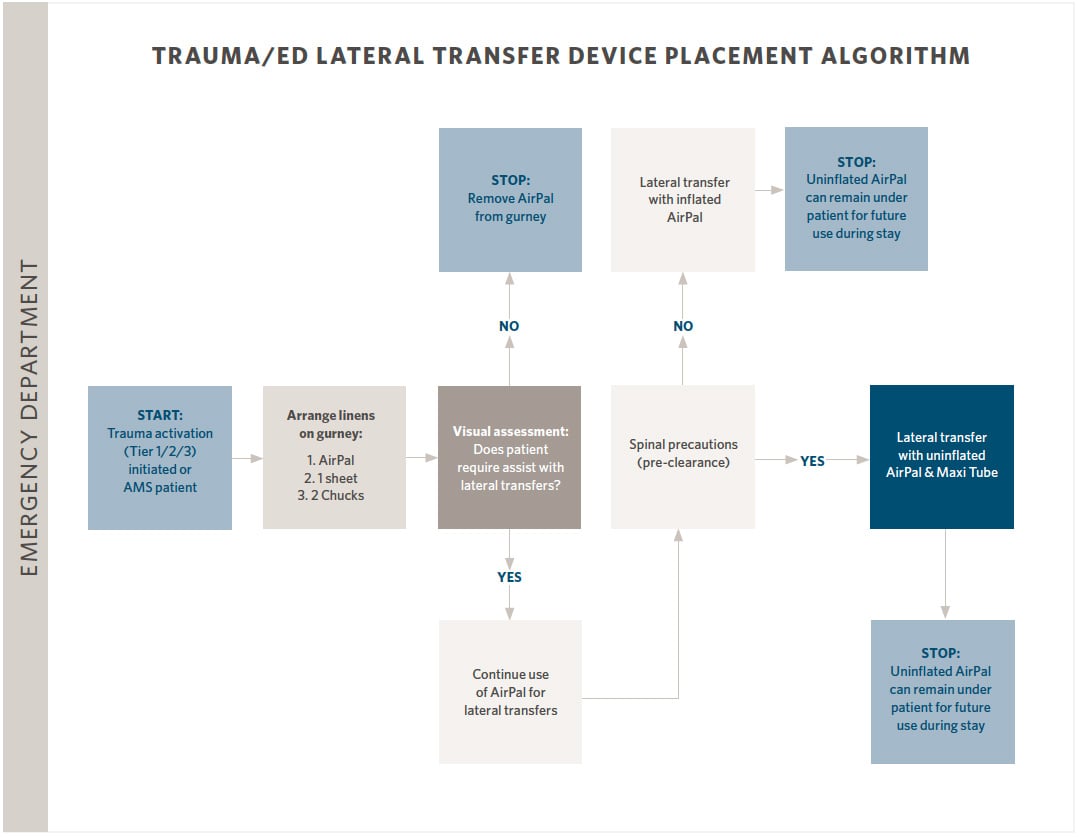
By establishing a standard that trauma patients will be placed on an AirPal, the AirPal system can be on the ED stretcher prior to patient arriving, preventing re-positioning the patient to place the mattress under the patient. The early implementation of AirPal allows safe patient transfers to take place from the time of admission through the entire course of the patients hospital stay. Having the mattress available, on the gurney, with an Air Pump in its designated location, ensures that utilization of AirPal and compliance of these safe patient-handling practices remains high.
“Up Sooner Safer has changed the dynamics of the CT Department, in two different areas; for employees and patients, both physically and mentally. It is so much easier on staff and patients. It has improved patient care and comfort while easing the physical burden on staff.
Kari Valdez, Lead CT Technologist
“CT department staff report that patients requiring repeated imaging, request that the AirPal be used every time.”
Travis Eckard, DPT, Up Sooner Safer Program Coordinator
Results
Reduction in HAPI occurrences is an ever-challenging endeavor in the acute care setting. Intuitively, improving patient mobility should have an effect on HAPI incidence. In the development of Up Sooner Safer, HAPI was not at the forefront of measures to look at program effectiveness. Hospital leadership began to see a direct correlation with Up Sooner Safer and HAPI rate soon after launch. Kern Medical was able to show a drastic reduction in reportable HAPIs since the launch of Up Sooner Safer. This reduction was not solely due to Up Sooner Safer. Kern Medical made a concerted effort to invest in its advanced wound care program. The combination of a strengthened advanced wound care program and following Up Sooner Safer policy and procedures resulted in a sustainable, average annual reduction of reportable HAPI incidence of 81%. (see Graph 2)
“Up Sooner Safer has been a great complement to our advanced wound care program. In combination with our advanced wound care team, it has helped maintain our low HAPI incidence.”
Joe Salvador, FNP-C, CWOCN, CWS
Graph 2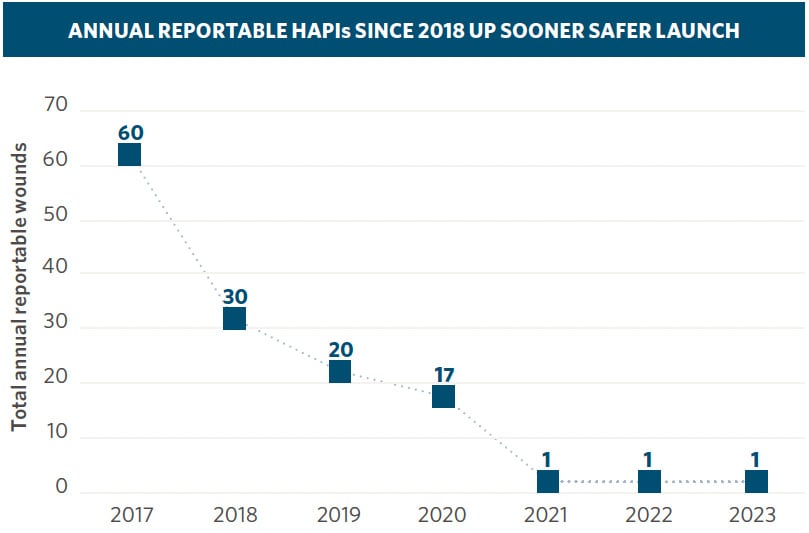
An analysis of the data reveals a significant reduction in employee patient handling injuries, lost employee days and average patient handling injury cost. The three-year average SPH employee injuries prior to Up Sooner Safer implementation was 11, a six year decline since program launch demonstrated a decrease by 75% with an average annual SPH patient handing occurrence of 2.8 injuries per year. (see Table 1)
While SPH injuries have not been eliminated, the severity of injuries has been drastically reduced when looking at the average number of lost days due to SPH injuries and cost per injury. Prior to 2018, the annual average of lost SPH employee injury days was 152 days; the average annual days lost between 2018-2023, and was six days per year. Additionally, the SPH injuries pre-2018 had an average worker’s compensation cost of $55,921 per injury; between 2018-2023, the average worker’s compensation cost was $5,755. (Data Table 1)
Table 1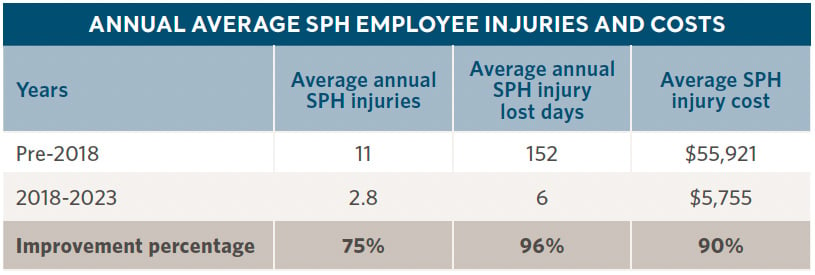
Discussion
Up Sooner Safer, is a SPH progressive mobility program that has positively impacted patients, employees and the organization. While SPH employee injuries continue to decrease and are less severe as seen by a significant decrease in lost employee days post-injury and reduction in worker’s compensation costs. Kern Medical was fortunate to have received a grant to aid in the development and implementation of Up Sooner Safer, but analysis has shown a significant return on investment with thoughtful, deliberate program development. Collaborating with the Arjo MOVE Program has resulted in a sustainable, model program incorporating safe patient handling and progressive mobility.
Continuous improvement
As time has passed, Kern Medical has found that continual system review is needed for Up Sooner Safer. Looking to staff for real-time feedback to determine what is working, where the gaps are in service, incorporating new technologies and refinement to better meet the needs of patients and staff. Kern Medical looks forward to continued potential partnership with Arjo in mobilizing patients, pressure injury and fall prevention.
Download case studies
Rooted in clinical evidence and driven by your facility data, Arjo MOVE supports you to deliver high quality care that facilitates patient and resident mobility, resulting in improvements in clinical outcomes, staff well-being, operational efficiency, and financial optimization.
Arjo MOVE - Guaranteed Outcomes Program
If you're interested in learning more about our Caregiver Injury Reduction, Pressure injury Prevention and/or our Falls Programs, we would be happy to support you with guaranteed results.
References:
- Berlowitz D, VanDeusen Lukas C, Parker V, et al. (Content last reviewed October 2014.) Preventing Pressure Ulcers in Hospitals: A Toolkit for Improving Quality of Care. Agency for Healthcare Research and Quality, Rockville, MD. Retrieved from http://www.ahrq.gov/professionals/systems/hospital/pressureulcertoolkit/index.html.
- Bauer K, Rock K, Nazzal M, Jones O, Qu W, “Pressure Ulcers in the United States’ Inpatient Population From 2008 to 2012: Results of a Retrospective Nationwide Study,” Ostomy Wound Management, November 2016.
- Padula WV, Delarmente BA. The national cost of hospital-acquired pressure injuries in the United States. Int Wound J. 2019 Jun;16(3):634-640. doi: 10.1111/iwj.13071. Epub 2019 Jan 28. PMID: 30693644; PMCID: PMC7948545.
- Gefen A (2018) The future of pressure ulcer prevention is here: Detecting and targeting inflammation early. EWMA Journal 2018, 19(2):7-13.
- Gefen, A (2008). How much time does it take to get a pressure ulcer? Integrated evidence from human, animal and invitro studies. Ostomy Wound Manage. 2008b; 54(10): 26-8,30-5.
- Dealey C, Posnett J, Walker A. (2012) The cost of pressure ulcers in the UK. Journal of Wound Care, 21 (6): 261-266.
- Costello, K. An evaluation of lateral patient transfer devices; CareGiver Ergonomics, 2021.
- McCoskey,K.L., Ergonomics and Patient Handling. AAOHN Journal, 2007, 55(11): 454-462.
- Gucer, P.W., Gairens, J., eta al. Sit Stand Powered Lifts in Long Term Care and Resident Quality Indicators. Jpurnal of Occupational Environmental Medicine. 2013 Jan; 55 (1): 33-46.