’Reduce the pressure and don’t sweat it!’ – Verticalization Therapy
(-Sharon Maris RN, Dominic Baily MIET, Carroll Gillespie RN, BSN, MS, CWOCN)
In critically ill patients, prolonged bed rest and immobility can lead to severe physical deconditioning, significant loss of muscle mass, and increased muscle weakness1. Verticalization therapy is utilized as a component of early critical care recovery protocols.

Abstract
Background
In critically ill patients, prolonged bed rest and immobility can lead to severe physical deconditioning, significant loss of muscle mass, and increased muscle weakness1. Verticalization therapy is utilized as a component of early critical care recovery protocols. In addition, the challenge of skin tissue breakdown as a result of intense and/or prolonged exposure to sustained deformation2, and insufficient management of microclimate between the skin and support surface, contributes to the development of pressure injuries2. These challenges co-exist and consideration of their combined management should form part of the overall patient risk assessment.
Purpose
This work explores the possibility of combining progressive standing and weight bearing using a tilting bed platform (figure 1), as an intervention to aid rehabilitation early in the acute phase of critical illness, while forming part of a pressure injury prevention strategy as it moves through various angles of incline. With the addition of a coverlet designed to influence skin/surface microclimate (figure 2), its impact was measured as a method to improve the overall surface performance of the bed system.
Methodology
Laboratory support surface performance characteristic testing, using pressure mapping and S3I testing apparatus³ was performed on a tilting or verticalization bed system with integrated support surface, to investigate the support surface performance in reactive mode. All testing was then repeated with a microclimate coverlet over the support surface to measure its impact. Finally, all indicative results were documented.
Pressure Area Index (PAI) testing
- Some deviation in protocol as the testing was completed with a human subject 183 cm Height, 80 kg weight, BMI 23.9 on the bed frame/support surface in the flat position 0° then at 45°, 60° and 82° angle of incline (verticalization).
- A flexible sensor pressure mat (X-Sensor X3 – Figure 3) was placed beneath the participant in order to quantify and visualize the pressure between the two contacts (participant and support surface).
ANSI RESNA SS-1 (Section 4) Sweating Guarded Hot Plate (SGHP) testing
A heated, moist indenter was applied to the support surface (with standard hospital sheet), analogous to the greater trochanter.
- Evaporative capacity was recorded – the indenter measures the resistance to flow of heat and moisture at 0° flat position.
ANSI RESNA SS-1 (Section 5) Horizontal Stiffness (Shear) testing
A pelvic indenter representing the trunk and pelvic area of a 50th percentile male was displaced laterally at 3 locations on the secured support surface in the 0° flat position, towards the foot end simulating patient movement. A recording of the force over time was captured.
- Average static force – which has to be overcome in order for movement to occur (indenter is displaced).
- Dynamic force – once movement begins at pre-determined time intervals.
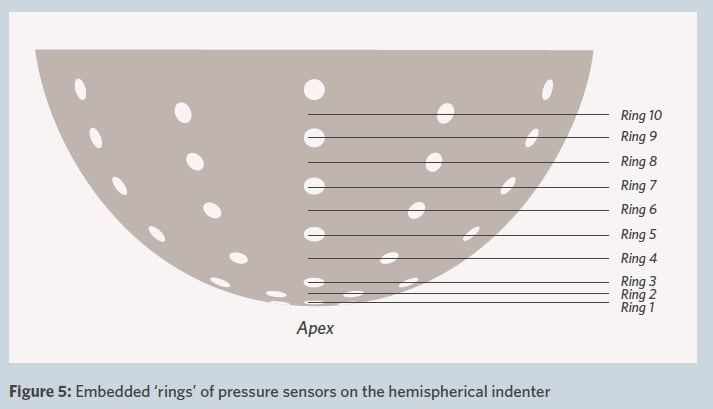
ANSI RESNA SS-1 (Section 6) Envelopment and Immersion testing
A hemispherical indenter (Figure 4) loaded to represent a 50th percentile male was used to measure the performance metrics on a 0° flat surface.
- Envelopment percentage – is calculated using contact depth / immersion depth.
- Immersion depth – using a laser distance sensor to measure the depth insertion of the test indenter into the support surface.
- Contact depth – using the ‘rings’ of 61 pressure sensors embedded within the test indenter, the depth of contact between the hemispherical indenter and the support surface can be measured. (Figure 5)
- Peak Pressure – using the embedded pressure sensors, the peak (or maximum) interface pressure at any point across the hemisphere can be measured (figure 5).
Verbal feedback
The participant was asked about the change in support being provided by the support surface during the various angles of verticalization.
Results
PAI metrics described in the test methods were tabulated for the verticalization bed system with integrated support surface both with and without the microclimate coverlet, and shown at the various angles.
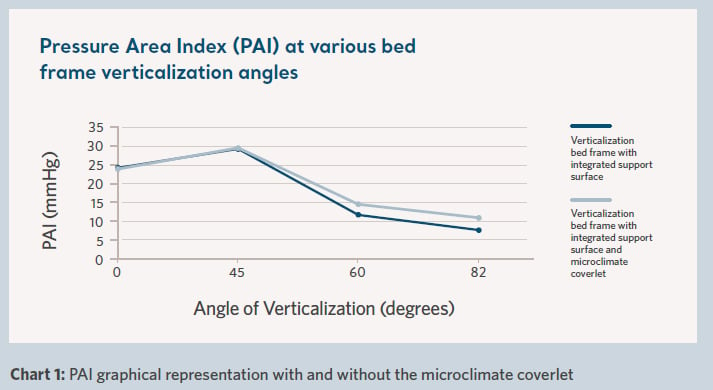
Clinical relevance of PAI testing – support surfaces which provide a higher patient contact area and a lower pressure area index are likely to provide better levels of pressure redistribution as they distribute the load across a larger surface area of the body.
ANSI RESNA SS-1 (Section 4) Sweating Guarded Hot Plate (SGHP) results are shown graphically in Chart 2.
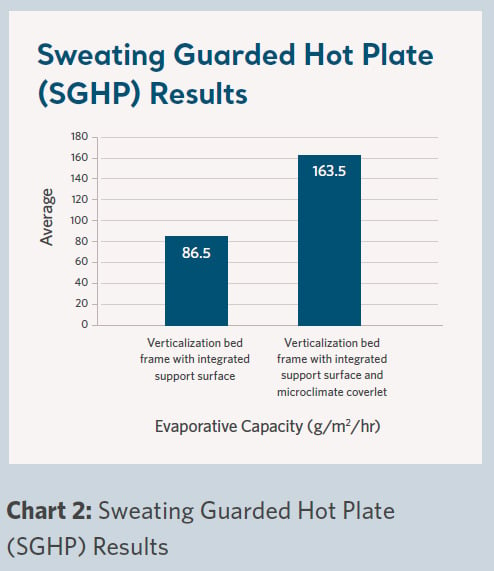
Clinical relevance of Sweating Guarded Hot Plate (SGHP) testing – to provide insight on the support surfaces rate of heat removal. The higher the number the more heat can be pulled away. A second outcome of this test is evaporative capacity, which provides insight into the ability of a support surface to remove moisture away from the body, the higher the number the more moisture may be removed from the surface of the patient’s skin, which can influence the patient’s microclimate.
ANSI RESNA SS-1 (Section 5) Horizontal Stiffness (Shear) testing results are shown
in charts 3 and 4. Positions 2, 3 and 4 are governed by the standard3.
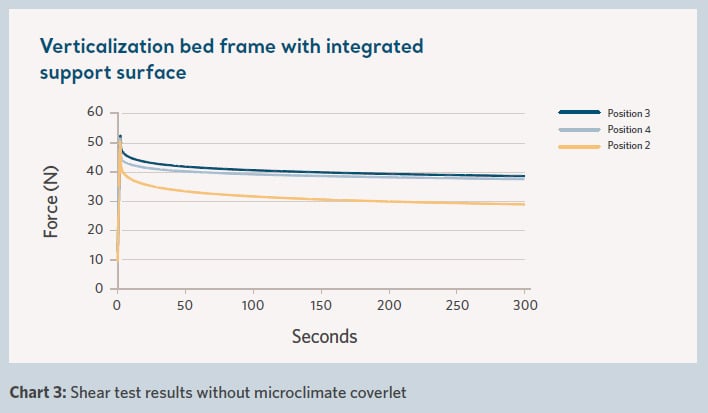
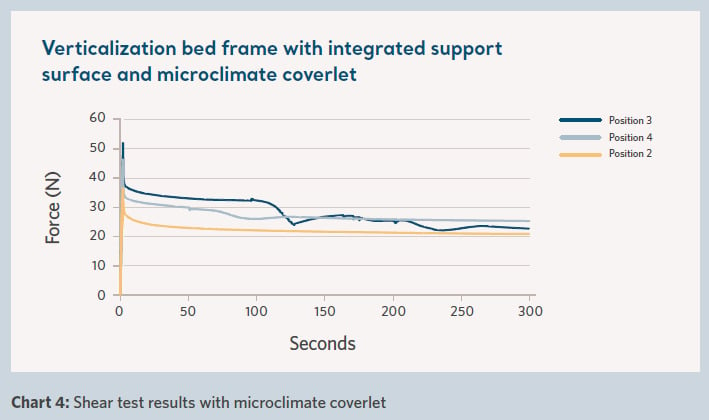
Clinical relevance of Horizontal Stiffness (Shear) testing – designed to simulate force that the support surface imparts on the individual as they slide towards the foot of the bed. The force is comparable to forces during repositioning and in bed movement. The guidance4 discusses the significance of higher forces which may reduce the patient migration down the bed, but may lead to tissue damage, versus lower forces resulting in a reduced ability to maintain patient position in the bed. All factors are to be considered as part of support surface selection and utilizing other methods of patient migration reduction.
ANSI RESNA SS-1 (section 6) Envelopment and Immersion contact depth between the hemispherical indenter and the support surface was equivalent at 38.1 mm both with and without the coverlet. The envelopment and immersion results are graphically represented in charts 5 & 6 below.
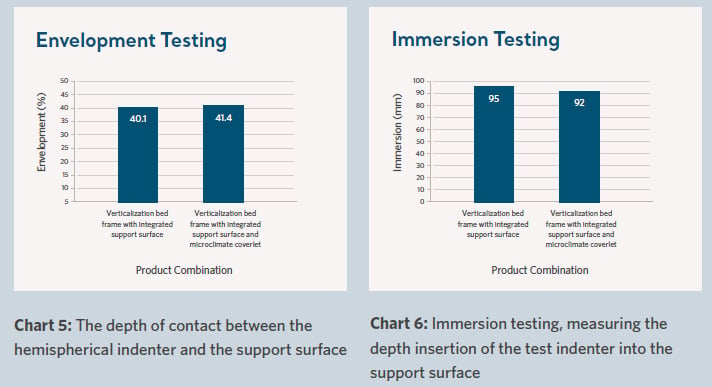
Clinical relevance of Envelopment and Immersion testing – a higher level of envelopment suggests how well the support surface conforms or molds around irregularities in the body, and immersion, the depth of penetration or sinking into the support surface, both providing an opportunity for increased pressure redistribution. The guidance4 around excessive immersion and limited immersion should also be considered as part of the individuals support surface selection requirements.
Results interpretation
- The PAI peaked at 45 degrees in the study and then a rapid drop is noted as the angle of verticalization increased. This was consistent with verbal feedback from the participant, who stated at approximately 50° the support was no longer being provided by the support surface, suggesting off-loading, and had now moved downward to their feet on the footboard. The data also showed no detrimental impact with the addition of the microclimate coverlet on the PAI throughout the measured angles of incline 0°, 45°, 60° and 82°.
- Adding the microclimate coverlet resulted in an 89% increase in the evaporative capacity, indicating a greater amount of heat and moisture removal from the patient/support surface interface, which may influence the patient’s microclimate and decrease risk of pressure injury development.
- A reduction in shear was noted to be approximately 25% with the addition of the microclimate coverlet, suggesting less force would be imparted on the individual by the support surface during repositioning and in bed movement.
- The envelopment and immersion data showed no detrimental impact with the addition of the microclimate coverlet, representing a consistent performance capability for pressure redistribution.
Conclusion
Skin protection considerations remain a priority when utilizing verticalization therapy during early rehabilitation in the acute phase of critical illness. Patients who require graded transition from bed rest to supporting their full body weight, can be progressively moved to a standing and weight bearing position as early and frequently as tolerated. Results from this study indicate, if verticalization therapy is tolerated and angles of incline above 45 degrees are achieved, this has an increased positive impact on pressure redistribution.
With the addition of a microclimate coverlet the evaporative capacity performance almost doubled, indicating a greater amount of heat and moisture removal, which may influence the patient’s microclimate. Combined with a 25% shear reduction, less force is imparted on the individual by the support surface during repositioning and in bed movement.
This exploratory work using performance characteristic testing metrics demonstrate that utilizing this combination of technologies for verticalization practice, has a positive impact on support surface performance and should be a consideration when risk assessing patients to minimize deformation (pressure/shear) and influencing the patients microclimate as part of a pressure injury prevention strategy during critical illness.
Download the document
Get personalized advice & solutions
References
- Mendez-Tellez PA, Nusr R, Feldman D, Needham D. Early Physical Rehabilitation in the ICU: a review for the neurohospitalist. Neurohospitalist 2012; 2: 96–105.
- European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel, Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers/Injuries: The International Guideline 2019. Emily Haesler (Ed.). 2019. Section 2 Etiology.
- ANSI/RESNA SS-1:2019. American National Standard for Support Surfaces – Volume 1: Requirements and Test Methods for Full Body Support Surfaces. 2019.
- NPIAP S3I Guidance on Interpretation of Performance Standards for Support Surfaces V2. 2020.