The power of intervention in pressure ulcer prevention and management
by Sharon Maris, Director Global Medical Affairs for Pressure Ulcer Prevention
Pressure ulcer prevention interventions are key to reducing the risk of developing painful, resource intensive and costly pressure ulcers.
As an industry supporter of Stop Pressure Ulcer Day, we are committed to empowering clinicians to improve outcomes in pressure ulcer prevention with a range of options to enable effective intervention, from support surfaces and repositioning systems to pressure ulcer prevention programs.
Of course, all interventions to prevent pressure ulcers must be led by the latest evidence-based guidance and coordinated by the multidisciplinary team.
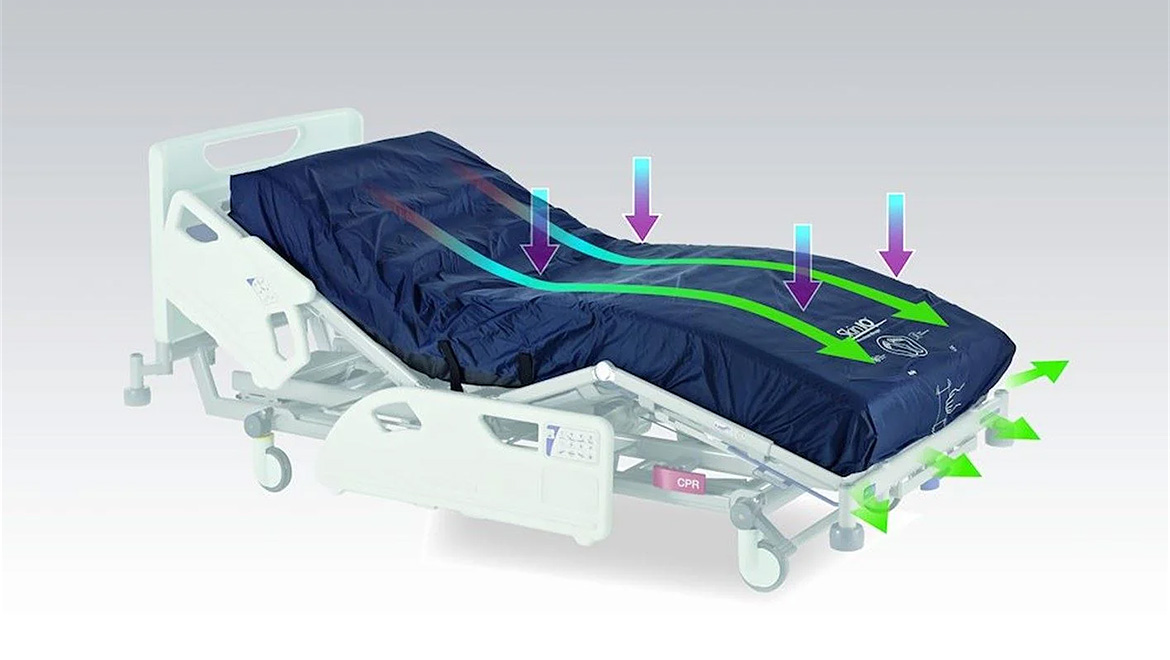
Intervention with support surface technologies
If we are to truly individualise pressure ulcer prevention and management, we cannot assume one product will fit all patient needs. Caregivers require access to a broad range of support surface technologies, which can be suitably matched against a patient’s condition and needs outside of the pressure ulcer risk we see captured during the risk assessment process like the Braden Scale or Purpose T.
As an example, once the patient is identified ‘at risk’ following assessment, and has existing skin damage, good clinical judgement may inform us that they require longer periods of targeted off-loading to a specific anatomical area. For this reason, the product performance characteristics of the support surface selected should match this.
Alternatively, if the assessment indicates the individual has a problem managing moisture at the skin/surface interface (microclimate) – resulting in an increased vulnerability due to its strong connection with frictional properties and shear¹ – a product with a higher moisture vapour transfer rate (MVTR) may be indicated.
Learn more about Arjo’s support surfaces and microclimate management products here
Intervention with repositioning systems
For those with little or no mobility who require regular repositioning intervention, caregivers should consider the techniques and equipment being used to reduce friction and shear, associated with unintended dragging during repositioning¹. This may include the use of friction reducing slide sheets or slide sheets in combination with patient lifts and slings.
The facility’s patient handling equipment can play an important part in the overall pressure ulcer prevention strategy, in addition to improving comfort and dignity during repositioning practices.
Learn more about Arjo’s patient handling systems here
Empowering clinicians with the ability to strengthen intervention strategies and elevate the pressure ulcer prevention pathway
Arjo Mobility Outcome Value Engagement (MOVE) programs are designed to arm clinical staff with the tools and knowledge to drive improvement towards both clinical and operational goals.
The MOVE Pressure Ulcer Prevention Programme is driven by facility data, combined with education and our expertise, to work in partnership to embed cultural change to achieve reduction in hospital acquired pressure ulcers (HAI’s).
Learn more about Arjo’s MOVE programs here
Stop Pressure Ulcer Day 2024
The awareness day in November each year aims to educate the public, professionals and politicians about pressure injures and how to prevent them.
This year’s theme ‘Are you really looking, are you really listening’, drives us to think about our communications on pressure ulcer. As clinicians, we need to consider the needs of our patients and colleagues as information can be overwhelming and difficult to process, therefore we might need to adjust or simplify our messages.
Raising awareness and reflection
My first thought on this year’s theme turns to the SSKIN bundle which has been around now for many years and used globally in multiple care environments from acute care hospitals to community and long-term care settings. The original bundle focused on 5 interventions for the prevention and management of pressure ulcers.
In the UK, NHS Improvement³ extended the framework of interventions to ASSKING, complimenting the core acronym with two fundamentals of care delivery, assessing and giving information:
A – Assess risk
S – Surface to ensure the patient has the appropriate support
S – Skin inspection to look for signs of early skin damage and provide skin care
K – Keep moving to reduce the impact of immobility on the skin
I – Incontinence and moisture management to keep the patient clean and dry
N – Nutrition/hydration, ensure adequate nutrition and plenty of fluids
G – Giving information
Just like this year’s theme for Stop Pressure Ulcer Day, both the SSKIN and AASKING bundles are driven by the need to adjust and simplify communication and education to make sure action or intervention occurs.
Clear, concise and easy to remember, these bundles ensure healthcare professionals, patients and their families have a fundamental understanding of the applied interventions to prevent and manage pressure ulcers.
On the topic of completing Risk Assessment Tools (RATs) e.g. Braden or Waterlow, these are usually performed to identify individuals at risk of developing a pressure ulcer⁴, however, there’s no reliable evidence to suggest that the use of structured and systematic pressure ulcer risk assessment tools reduce the incidence, or severity of pressure injury when compared to risk assessment using clinical judgement⁵.
Current guidelines¹ recommend that use of clinical judgement is essential and overarches the risk assessment score.
Often discussed is what we mean by clinical judgement. It refers to the process by which nurses make decisions based on nursing knowledge – evidence, theories, ways/pattern of knowing and other disciplinary knowledge, critical thinking and clinical reasoning. Clinical judgement is directly related to care outcomes⁶.
In summary, combining the RAT outcome along with clinical judgement is essential for planning intervention for pressure ulcer prevention.
However, we must be mindful it’s the execution of planned interventions built into the individual’s clinical care pathway that remain fundamental to positive patient outcomes.
Download
Support surface and patient handling intervention in pressure ulcer prevention, and measuring outcomes that matter – utilising international clinical practice guidelines as part of the pressure ulcer prevention strategy Download here
Watch the webinar
Pressure Injury/Ulcer Prevention: Understanding the Science of Support Surfaces, with Michele Deppisch, Wound Care Consultant and Vice Chair for the Support Surface Standards Initiative (S3I) committee Watch the webinar
Contact an expert
References
- European Pressure Ulcer Advisory panel, National Pressure Injury Advisory Panel, Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline. The International Guideline. Emily Haesler (Ed). EPUAP/NPIAP/PPIA: 2019
- Li Z, Lin F, Thalib L, Chaboyer W (2020). Global prevalence and incidence of pressure injuries in hospitalised adult patients: A systematic review and meta-analysis. Int J Nurs Stud 105: 103546
- NHS Improvement. Pressure ulcer core curriculum. Publication code SL 10/18. NHS Improvement, London. 2018.
- Weller, CD, Gershenzon, ER, Evans, SM, Team, V, McNeil, JJ. Pressure injury identification, measurement, coding, and reporting: Key challenges and opportunities. Int Wound J. 2018; 15: 417– 423.
- Moore ZEH, Patton D. Risk assessment tools for the prevention of pressure ulcers. Cochrane Database of Systematic Reviews 2019, Issue 1. Art. No.: CD006471.
- Clinical Judgement concept tool kit. American Association of Colleges of Nursing (AACN). 2022


_Blog%20Image.jpg)